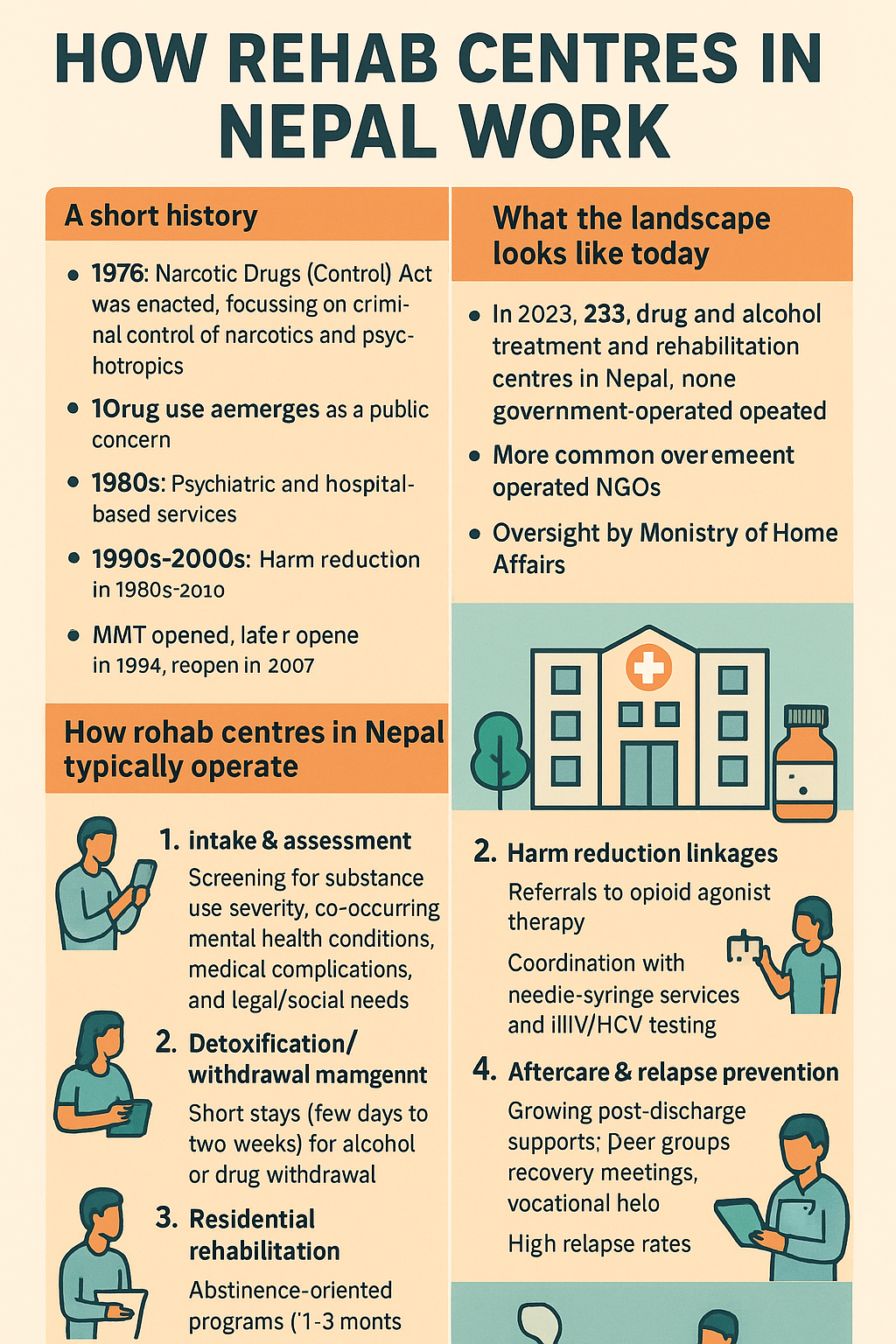
A short history: from punitive control to mixed-care responses
Legal foundation (1976): Nepal’s modern drug policy began with the Narcotic Drugs (Control) Act, 2033 (1976), which focused on criminal control of narcotics and psychotropics. This law still underpins regulation and enforcement today. Siddhasthali Rural Community Hospitalphrdnepal.org.np
Drug use emerges as a public concern (1960s onward): UN profiles note that “modern” drug abuse in Nepal dates to the 1960s as contact with the outside world expanded. UNODC
Psychiatric and hospital-based services (1980s): Dedicated psychiatric services at Tribhuvan University Teaching Hospital opened in 1986–87, laying groundwork for clinical addiction care within hospitals. PMC
Harm reduction enters (1990s–2000s): Methadone Maintenance Treatment (MMT) first launched in 1994, was shuttered in 2002, and reopened in 2007—a pivotal shift from a purely punitive lens to a health-oriented approach for opioid dependence. ScienceDirect
Peer-led recovery (2001–present): The civil-society network Recovering Nepal began in 2001 as a grassroots support group for people who use drugs (PUD) and those living with HIV/TB, later growing into a national advocacy and service platform. Recovering Nepal
What the landscape looks like today
How many centres? Who runs them? A 2023 review estimated ~235 drug and alcohol treatment and rehabilitation centres, none government-operated, reflecting heavy privatization and NGO leadership. Oversight largely sits with the Ministry of Home Affairs, not the health ministry—an unusual arrangement by global standards. SpringerLink
Burden of use: The Government’s Nepal Drug Users Survey 2019/2020 counted 130,424 people who use drugs (about 93% male). Media summaries and WHO documents frequently cite these figures. Police anticipated the number could double by the next survey cycle. Nepal in DataKhabarhubKathmandu PostWHO
Harm reduction & funding: Needle–syringe programs and opioid agonist therapy (e.g., methadone/buprenorphine) exist but coverage has historically been limited; financing relies heavily on the Global Fund/Save the Children and partners rather than domestic budgets. Harm Reduction International
System strengthening: WHO and partners have recently funded work to strengthen de-addiction services (e.g., 2023 TORs for scaling alcohol and substance use care). WHO+1
How rehab centres in Nepal typically operate
While models vary by provider and province, most centres offer versions of the following:
Intake & assessment: Screening for substance use severity, co-occurring mental health conditions, medical complications, and legal/social needs (often with limited standardized tools). (General practice contextualized by Nepal reviews.) PMC
Detoxification/withdrawal management: Short stays (often a few days to two weeks) for alcohol or drug withdrawal; medical oversight quality can vary, particularly in small private facilities. (Landscape review and Nepal studies.) SpringerLinkPMC
Residential rehabilitation: The most common model—abstinence-oriented programs (often 1–3 months), group counseling, 12-step facilitation, basic psychoeducation, life-skills training, and family sessions. Evidence-based psychotherapies (CBT, relapse prevention) are present in some centres but not uniformly. (Nepal literature reviews and centre audits.) PMC
Harm reduction linkages (select sites): MMT/OST referrals for opioid use disorder; some centres coordinate with needle–syringe services and HIV/HCV testing. Coverage remains patchy. ScienceDirectHarm Reduction International
Aftercare & relapse prevention: Post-discharge supports—peer groups, recovery meetings, vocational help—are growing but formal, evidence-based aftercare is limited, and relapse rates remain high in the first months post-treatment, underscoring the need to scale structured relapse-prevention approaches. PubMedPMC
Key developments over time
Shift toward harm reduction: The reintroduction of MMT in 2007 and integration with HIV prevention signaled a more health-centred approach for high-risk populations. ScienceDirect
Civil society leadership: Networks like Recovering Nepal (since 2001) have professionalized peer support, advocacy for human rights-based drug policy, and community recovery services. Recovering Nepal
Scale without state operation: The rapid growth to ~235 centres by early-mid 2020s happened largely outside direct government provision, creating wide variability in quality and emphasizing the need for licensing, standards, and clinical governance. SpringerLink
International and UN engagement: UNODC and global partners have framed Nepal’s drug trends and interventions since the 2000s, while recent WHO activities target system strengthening and quality improvement. UNODC+1WHO
Ongoing gaps and priorities
Move stewardship to the health sector: Many experts recommend aligning addiction care under the Ministry of Health and Population for clinical standards, workforce development, and integration with primary care—rather than the current Home Affairs lead. SpringerLink
Expand evidence-based care: Broader access to OST, CBT/relapse-prevention, and integrated mental health services can reduce early relapse and improve outcomes. ScienceDirectPubMed
Strengthen aftercare & community recovery: Nepal-based reviews repeatedly flag limited structured aftercare—a key driver of relapse. Scaling peer-led recovery, vocational pathways, and family-based supports is essential. PubMedPMC
Sustainable domestic financing & standards: Reliance on external grants for harm reduction makes coverage fragile. National standards, accreditation, and routine data can lift quality across the many private/NGO centres. Harm Reduction International
Quick reference (dates & milestones)
1960s: Modern drug abuse becomes visible in Nepal. UNODC
1976: Narcotic Drugs (Control) Act enacted. Siddhasthali Rural Community Hospital
1986–87: Psychiatric services established at TUTH (foundation for clinical addiction care). PMC
1994: Methadone program launched; 2002 closure; 2007 relaunch (OST/harm reduction era). ScienceDirect
2001: Recovering Nepal begins as a peer support network; later a national platform. Recovering Nepal