We’ve all heard it before: “Addiction is a choice.” “If they just had more willpower, they could stop.” This stigma is not only harmful—it’s scientifically wrong.
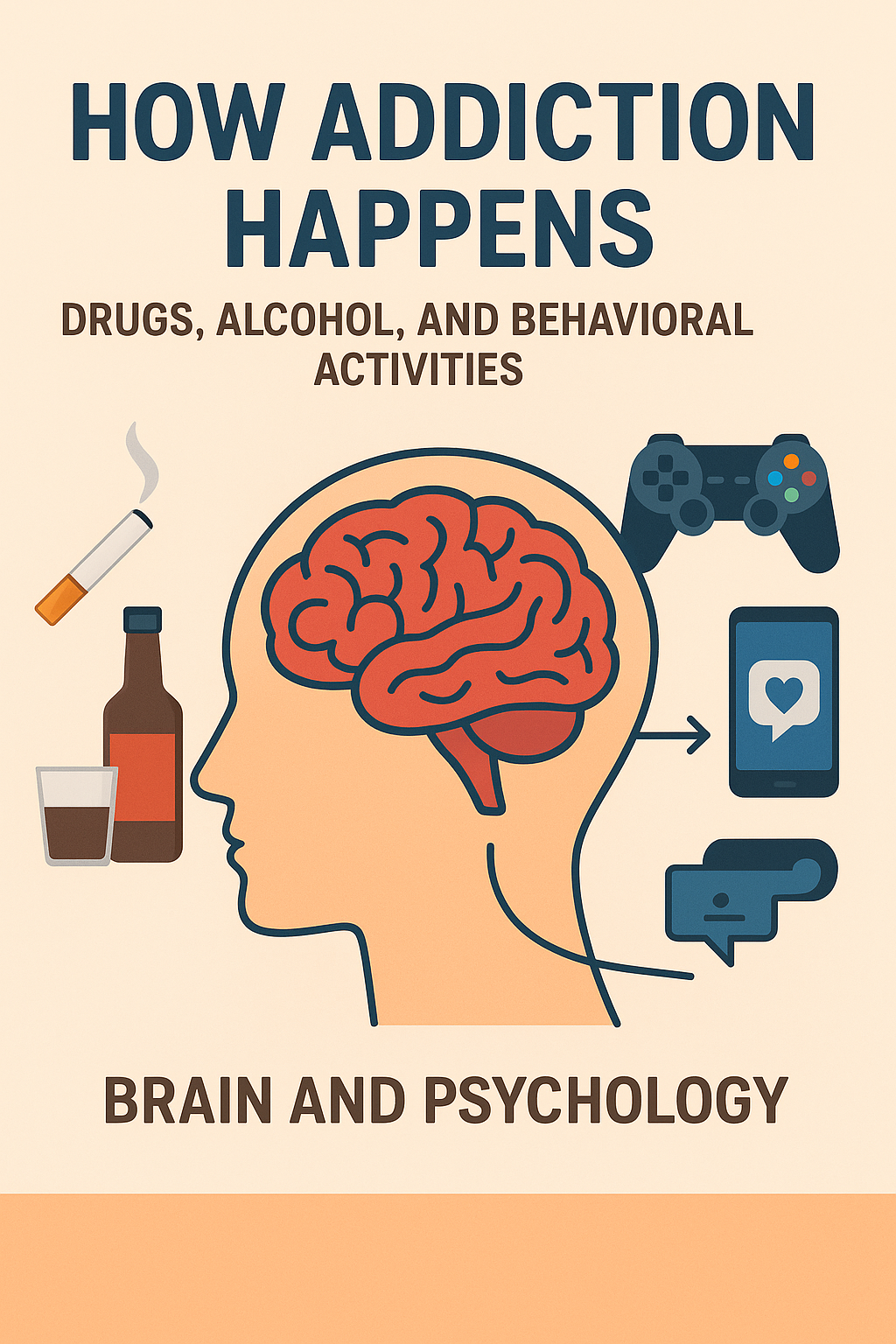
Modern neuroscience reveals a far more complex story. Addiction, whether to substances like drugs and alcohol or behaviors like gambling and gaming, is a chronic brain disorder. It fundamentally alters our brain’s wiring, hijacking the very systems designed to keep us safe and happy.
Let’s break down how addiction happens, moving beyond the myth of moral failure to understand the powerful biological and psychological forces at play.
It’s a Brain Disease: Addiction physically changes the brain’s structure and function, particularly its reward and impulse-control centers.
It’s Not Just Substances: Behaviors like gambling, gaming, and social media use can trigger the same addictive pathways as drugs or alcohol.
The Cycle is Powerful: Addiction creates a self-reinforcing loop of tolerance, dependence, and compulsive use despite negative consequences.
Recovery is Possible: Understanding the science behind addiction paves the way for effective, compassionate treatment strategies.
The Star of the Show: Your Brain’s Reward System
To understand addiction, you first need to meet your brain’s reward circuit. This network, which includes areas like the nucleus accumbens and prefrontal cortex, is designed to make you feel good when you do something necessary for survival—like eating or socializing.
The key player here is dopamine, a neurotransmitter that creates feelings of pleasure, motivation, and reinforcement. It’s your brain’s way of saying, “That was great! Do it again!”
Addiction hijacks this entire system. Substances and certain behaviors flood the brain with a surge of dopamine far greater than anything achieved naturally. The brain, overwhelmed by the chemical onslaught, starts to adapt.
How Substances Hijack the Circuit: Drugs and Alcohol
Drugs and alcohol force the brain to release massive amounts of dopamine or prevent its normal recycling, creating an intense but artificial euphoria.
Stimulants (e.g., cocaine, methamphetamine): Create a massive dopamine flood, leading to intense energy and euphoria.
Depressants (e.g., alcohol, opioids): Enhance calming neurotransmitters (like GABA) and also boost dopamine, leading to relaxation and pleasure.
This hijacking leads to a devastating cycle:
Tolerance: The brain, trying to regain balance, reduces its own dopamine production and receptors. The same amount of substance no longer produces the same high, leading users to consume more.
Dependence: The brain adjusts to functioning with the substance. Without it, withdrawal symptoms—both physical and psychological—emerge.
Addiction: Use becomes compulsive and uncontrollable. The individual continues despite severe harm to their health, relationships, and life.
Yes, You Can Be Addicted to Behaviors, Too
This isn’t just about substances. Behavioral addictions to activities like gambling, gaming, pornography, or even social media follow the same neural blueprint.
These activities trigger dopamine spikes—when you win a bet, get a “like,” or unlock a new achievement. The most addictive behaviors often use a “variable reward system” (the same principle behind slot machines). You don’t know when the reward is coming, so you keep compulsively checking, scrolling, or playing in anticipation.
Psychologically, these behaviors often become a maladaptive coping mechanism for stress, anxiety, or loneliness.
The Perfect Storm: Biology Meets Psychology
While the brain mechanism is universal, not everyone develops an addiction. Psychological factors create vulnerability:
Genetics: Family history can account for about 40-60% of a person’s susceptibility.
Mental Health: Conditions like depression, anxiety, and ADHD are significant risk factors, as individuals may self-medicate to relieve symptoms.
Stress and Trauma: Early life adversity or chronic stress can alter brain development and increase the risk of addictive behaviors.
Environment: Easy access to substances and lack of a strong support system play major roles.
Why It’s So Incredibly Hard to “Just Stop”
The most crucial area to understand is the prefrontal cortex—the brain’s CEO. This region is responsible for judgment, decision-making, and impulse control.
In addiction, this area becomes weakened and dysregulated. Meanwhile, the reward system, screaming for its next fix, becomes hyperactive. This means the part of the brain driving impulse is overpowering the part designed to control it. It’s not a lack of desire to quit; it’s a literal power imbalance within the brain itself.
The Path to Recovery: Rewiring the Brain with Hope
The good news? The brain possesses an incredible ability known as neuroplasticity—the power to heal and rewire itself. Effective treatment addresses both the biological and psychological aspects:
Medical Intervention: Detox and medications can manage withdrawal and cravings, helping to restore chemical balance.
Therapy: Cognitive Behavioral Therapy (CBT) helps individuals recognize and change destructive thought patterns. Therapy also provides new coping skills.
Community: Support groups provide connection, reduce shame, and offer accountability.
Healthy Rewards: Replacing addictive behaviors with healthy ones (exercise, hobbies, meditation) helps rebuild the brain’s natural reward system.
Final Thoughts: A Call for Compassion
Understanding addiction as a complex brain disorder changes everything. It moves the conversation from blame and punishment to empathy and treatment.
If you or someone you love is struggling, please know this: Addiction is not a moral failing. It is a health condition. And like other chronic conditions, with the right support and evidence-based treatment, recovery is not just possible—it’s within reach.
Resources:
Substance Abuse and Mental Health Services Administration (SAMHSA) National Helpline: 1-800-662-HELP (4357)
National Institute on Drug Abuse (NIDA): www.drugabuse.gov
Alcoholics Anonymous (AA) / Narcotics Anonymous (NA)
Leave a Reply